Look And Listen: Cognito And WVU Imagine A Future Beyond Alzheimer’s
What's that h-word again?
Cognito Therapeutics and West Virginia University’s Rockefeller Neuroscience Institute (RNI) have announced a strategic partnership that lays the groundwork for a new, neurotech-enabled learning healthcare system, initially focused on treating Alzheimer’s disease but aiming for much more.
The Brain Health Collaboratory is an ambitious initiative to advance science, medicine, and public health “by merging clinical care, AI-powered research, and continuous data generation.” The collaboration will harness Cognito’s treatment platform and RNI’s unique attributes to build a rural center of excellence for brain health innovation.
I spoke to Cognito’s CEO Christian Howell and RNI’s Executive Chair, Dr. Ali Rezai about their vision for this partnership and the broader headwinds driving progress in neurotechnology markets.

Cognito Therapeutics, founded in 2016 by neuroscientists Ed Boyden and Li-Huei Tsai, has raised over $200m in private capital to commercialize a novel disease modifying treatment. Spectris is the company’s headset, which delivers acoustic and light-based stimulation at a 40 hertz frequency for an hour per day.
Since earning FDA Breakthrough designation in 2020 for their device, Cognito completed a six-month early feasibility study with 76 patients, a subsequent voluntary 12-month extension to study longer-term outcomes, and kicked off their pivotal study, which is now fully-enrolled with 673 patients and anticipated completion in spring 2026.
Beyond demonstrating a promising safety profile and patient tolerability, Cognito has published numerous data suggesting their “neuroprotective” approach can help preserve cognition, brain function, and brain volume, while reducing health system costs.
“After 60 days of stimulation at 40 hertz, you can see what’s happening by looking at people’s spinal fluid, ” Howell told me. “We’re seeing significant protein expressions in synapses, myelin and cognitive resilience proteins. At 90 to 120 days under MRI, you can see not just myelin preservation, but those proteins actually having a restorative effect, building synaptic plasticity and improving glymphatic function. So in that way, validating mechanisms of action, understanding biomarkers, and that custody of evidence, our approach is much more in line with a biotech company.”
Mission, Vision, Decision
Howell was working at Medtronic when he met Rezai, at a time when former CEO Omar Ishrak challenged him to think about value-based care models at organizations like Geisinger and Mayo Clinic.
Rezai is a practicing neurosurgeon who has pioneered treatments in deep-brain stimulation, focused ultrasound, and other technologies, held leadership appointments at several prominent neurosurgical associations, and driven awareness of emerging treatments through appearances on 60 Minutes and other media.
Howell joined Cognito in 2023 and became CEO in August of last year, at which point he reconnected with Rezai. The two began exploring ways to advance a deeper understanding of the biological mechanisms of action in Alzheimer’s and other brain health diseases and ailments, while advancing clinical, economic, and social attributes of treatment at the population level.
The Collaboratory will live within RNI, which Rezai describes as “an eight year old startup” that “combines neurology and neurosurgery and psychiatry and radiology and rehab all under one unit.” RNI’s 47 practice locations and telehealth capabilities care for about 300,000 patients across a rural footprint of West Virginia, Southwestern Pennsylvania, Eastern Ohio, and Western Maryland.
“We take care of about 10,000 patients a year who have Alzheimer’s disease, about 9,000 with Parkinson’s. And we’re a payer provider as well with our insurance company,” said Rezai. “Our ecosystem has 330 different physicians and scientists in the neuroscience institute and about 2,400 team members. All of that allows us to really connect the dots. Having data connectivity and a digital footprint are important. All of them work on the same record system, with the same imaging standards for MRIs, EEGs, EMGs. The same team analyzes data. So we found this a very unique opportunity to study an in-home neurotherapeutic product, follow it longitudinally and advance the science behind it.”
Given the in-home nature of both the Spectris treatment and the acute impact of Alzheimer’s disease, a critical pillar of this initiative is caregiver engagement. “The family member burden is enormous in terms taking care of the patient and the entire family,” explained Rezai. “The emotional impact and financial impact on these people is very significant. In our system we have a caregiver program to address emotional and physical health, with counselors and other support provided free of charge.”
The center is co-funded by Cognito and RNI today, but will eventually draw upon external support, similarly to Rezai’s work in focused ultrasound, which has drawn state funds and non-profit grants in recent years. “As we get data that shows that we can change the course of Alzheimer’s potential with a home-based therapy, you’re looking at imaging data, biomarkers that we’re changing, and the health economics of that, I think that would lend itself to further government funding, NIH funding, other sources, foundations and donors.”
Looking ahead, Howell expects Cognito will forge “only three or four of these types of Collaboratories” given both the high bar for finding aligned health system leadership and the depth of involvement required for a venture-backed startup running a large pivotal trial.
Show & Tell: Beyond Clinical Evidence
Howell is clear that Cognito’s work in Alzheimer’s disease is far from complete, describing the initiative as not a commercial launch strategy, but a fully integrated partnership for holistic exploration.
While their HOPE pivotal trial aims to demonstrate clinical effectiveness to meet the FDA’s expectations, Howell speaks to the cost effectiveness and health economics that will be needed to meet the expectations of CMS and unlock a national coverage determination. Beyond reimbursement, Cognito’s goal is ensuring that when the technology is approved, it’s not just available, but it’s accessible, usable, and as effective as it can be for all stakeholders.
“In God we trust, and everyone else bring data,” Howell said. “The evidentiary burden for drugs is in the pre-market, and the evidentiary burden for devices is in the post-market. But the only way you can shift that burden in the post market to start with robust premarket evidence generation.”
Rezai describes the unique opportunity to understand the community-level impact of earlier and more effective therapy starting in West Virginia, rather than San Francisco, Boston, New York, or other large metropolitan areas where innovation typically starts.
“This is a big opportunity to show that we can help save people money, save visits, help caretakers not have to leave their jobs, take time off work, stay in the workforce. We want to see if this lightens the immense daily burden, the emotional burden and depression that comes with it. I mean, directly and indirectly, Medicare is paying so much money (on Alzheimer’s disease), and it’s astronomically growing.”
Is this the beginning of a value-based care model for Alzheimer’s? RNI’s system-level data on global costs will contribute to health economics and outcomes research (HEOR) to better understand comparative pricing strategies, patient and caregiver engagement, clinical education and training, and myriad other real-world priorities beyond what’s needed for reimbursement.
“I want to continue to show the value of that neuroprotective environment in less progressed disease and even potentially in the absence of disease,” Howell said. “We eventually want to be able to say, is this therapy something that we should be thinking about for more people? Is increasing plasticity and resilience something we should be thinking about proactively to address our brain health?”
So Good It Hertz: Ripples and Roadmaps
This partnership holds implications for the neurotech field and US healthcare far beyond new headsets and dementia care models.
Towards More Neurotech Adoption
With better treatment, patients may come in earlier. Though diagnosis remains a challenge at scale, additional neurotechnologies hold potential to bend the curve of how dementia impacts households, workplaces, and economies worldwide. Cognito already uses “confirmatory EEG testing” to identify the right cohort of patients, as per Howell. “Every data point we’ve seen tells me the earlier that someone can get diagnosed, not only are doctors and families better equipped to take on their disease, but it actually is more cost effective.”
Rezai is a rare health system leader who embraces the role of modern diagnostic and detection technology to usher in a new system-wide approach to identifying and supporting patients earlier in their journey. He described the RNI’s use of analytics, optical coherence tomography (OCT), gait analysis, blood and genetic testing, other technologies and signals, from eye movement to loss of smell.
“We look not just at Alzheimer’s, but neurodegenerative conditions across the board. So it’s Parkinson’s, vascular dementia, Alzheimer’s, Lewy body, frontotemporal, many areas,” he said. “It’s a whole group of conditions that have a lot of crossover. I mean, some have motor manifestations, some have cognitive behavior. It’s a spectrum. It’s about brain disease.”
RNI has also pioneered work in focused ultrasound with Insightec’s system for Alzheimer’s and opioid addiction, as well as brain-computer interfaces with Precision Neuroscience. This new Collaboratory model could incorporate additional neurotechnologies down the line. “We cannot really make something substantive at scale without industry partnerships,” Rezai said.
Pushing the Dialogue on Public Engagement
Howell has been actively discussing Cognito’s work with state level leaders and members of Congress. The FDA’s Center for Devices and Radiological Health (CDRH) has avoided the brunt of federal layoffs, but at a time of federal uncertainty, ensuring effective regulation and reimbursement remains a bipartisan priority.
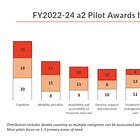
In describing a recent visit to Capitol Hill, Howell expressed confidence in the federal government’s fluency on emerging neurotechnologies and the details of medical device reimbursement for breakthrough devices through programs like TCET. He spoke to the importance of conducting larger scale studies in neurotech to build an evidence base beyond safety and clinical efficacy early on.
“There was a real acknowledgement of the need to make sure there’s coverage and reimbursement so that patients can access new treatments. If it’s clinically validated, not just conceptual, the senators made it clear they were happy to take that to the Secretary.”
Beyond bridging the valley of death, the next few years present a growing opportunity to connect clinical innovation to federal initiatives at the VA, ARPA-H, CMS, NIH, and other federal agencies. Neurotech industry leaders who are thinking beyond their next funding round could help usher in a national paradigm shift beyond pharmaceutical treatments that have shown limited effectiveness in psychiatry, neurology, rheumatology, and other specialties.
The Potential of Health System Partnerships
At Mount Sinai’s BCI Symposium last month, leaders from Mass General shared the launch of the nation’s first BCI clinic, “which aims to be a clinical center of excellence that coordinates care across specialties and technologies, starting before diagnosis and continuing through device implantation and ongoing care management. Beyond benefiting patients, families, and clinical teams, such a unified model could facilitate cost-effectiveness studies that could prove valuable to the industry in the coming years.”
RNI and Cognito’s new Collaboratory offers a similar model that other health systems could emulate, rooted in established clinical expertise, aligned incentives, visionary leadership, and emerging technologies. This initiative also expands the horizon for driving generational advances through braided funding from strategic philanthropy, venture capital, and public-private investments.
Earlier this month, Arena Bioworks announced it was abruptly shutting down, less than two years after launching with $500 million intended to support “a decade of scientific R&D.” Rather than freeing renowned researchers to advance science, the project burned through $200 million before crumbling due to lack of dedicated leadership, trust, and fears of a volatile biotech market, all before it accomplished anything.
While well intentioned, part of the issue may be that such bold, expensive endeavors, ostensibly aimed at advancing human health through open discovery, are fundamentally disconnected from patient care and the broader context of human life. A newer innovation model gaining momentum is the focused research organization, a non-profit seeded with $50-100 million dollars and tasked with advancing moonshot projects in five to seven years.
What happens after that time? No FRO has gotten there yet, so we don’t know. As Forbes Alex Knapp wrote in 2023, quoting former Google CEO Eric Schmidt, “FROs take on problems that might require a greater level of team science or systems engineering than is possible in an academic setting. Or they might aim at producing public goods that venture capital could not profit from.”
Could a Collaboratory model anchored with a visionary health system provide FROs like Forest Neurotech or open-source innovators like Openwater the right conditions to turn their innovations into sustainable and scalable flywheels of research and treatment?
Which Comes First: Care Model Or Foundation Model?
On a daily basis, I hear from new startups building “foundation models” to understand the human brain using EEG data collected from wearables, implanted sensors, or other data sourced from third parties. BCI leaders like Synchron have inked partnerships to advance these models, and many others are following suit.
With the hype around AI’s potential to “decode the human brain,” better understand cognition, cure diseases and transform healthcare growing by the day, I asked Rezai how their Collaboratory has actually been leveraging advanced AI capabilities.
“AI is sort of a loose term used for everything now these days, but it’s integrated into everything we do,” said Rezai. “We focus very heavily on that. It’s a mission for us that’s really important as a neuroscience institute in a rural community. So we’ve been following 6,000 patients in our ecosystem for the past five years, looking at people with severe addiction or Alzheimer’s, Parkinson’s, vascular dementias.”
He described heavy investments in infrastructure for digital disease management, longitudinal tracking across wearables, sleep tracking, heart rate variability, electronic medical record data on visits, telehealth visits, medications, patient survey apps for stress, anxiety, emotional health symptoms, for neurodegenerative care, addiction care, and beyond.
“So all that data goes into a large, continuous backbone of AI. The key thing is context with the data, linking to whether people are getting worse or getting better, or thriving. That’s why this comprehensive ecosystem is really important, because it should be neurologists, neurosurgeons, neuroimaging people, psychiatrists, blood biomarker analysts, the AI people, the software engineers, all those people working in this, and critically linking it to how the patient is. That context is absolutely mission critical. Otherwise, the AI systems are handicapped because they don’t have the clinical context.”
Howell added “What I really love about the RNI is that this is an institute that’s really proactively trying to understand the brain. They have a very robust neuroscience team that’s trying to understand base functionality, how is the brain operating, thinking about brain optimization beyond treating disease. And the fact that it all happens in the same ecosystem is unbelievably valuable for a company like ours because ultimately we’re starting with the underlying pathology of a disease, but our end goal is to address resilience.”
Originally published in Forbes Nov 13 2025



The partnership model here is really fascinatng. What stands out is how they're thinking beyond just FDA approval to the whole ecosystem of care delivery and caregiver support. The fact that RNI already treats 10,000 Alzheimer's patients anually creates a perfect testing ground for real world effectiveness. It's refreshing to se neurotech companies engaging with health systems early rather than waiting until post approval to figure out implementation challenges.